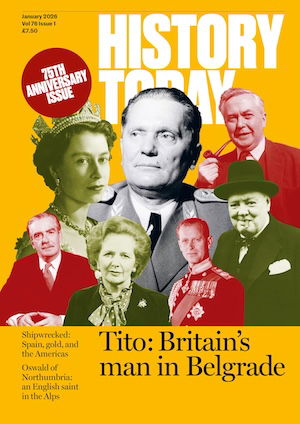
All’s Fair in Blood and War
The pain of war had at least one positive side-effect: medical advances in haematology.
It is an extraordinary paradox that war, the cause of so much havoc and misery, could be associated with important life-saving innovations in fields such as haematology. Yet the connections are protean and go back to the beginnings of history. Herodotus tells us that the Scythians drank the blood of their slain enemies, presumably predicated on the belief that blood contained the essence of their bravery, which could be transferred from the victim to the victor.
During the Enlightenment a number of experiments in blood transfusion were undertaken by fellows of the Royal Society and the French Academy of Science, although the idea of blood transfusion as a life-saving technique did not occur to them. Following a number of injudicious experiments – such as the transfusion of blood from a calf to treat mental illness, carried out by Jean-Baptise Denys, which resulted in the death of the patient – the practice of blood transfusion was deemed to be a criminal act by the French parliament. Shortly afterwards, the Royal Society began to distance itself from blood transfusion and Pope Innocent XI banned it.
One of the greatest advances was the identification of three major blood groups by Karl Landsteiner in 1901, for which he received a Nobel Prize. Six years later, Jan Jansky, a Czech neurologist, psychiatrist and serologist, accurately described four major blood groups (now identified as A, B, O and AB). He received little credit.
The discovery of blood groups was an essential forerunner to modern blood transfusion.
By the 19th century the idea emerged that blood transfusion might have a role to play in saving the lives of women from post-partum haemorrhage. Yet, despite developments in the knowledge of blood groups and prevention of blood clotting, blood transfusion was not widely adopted during the First World War. This was in spite of the fact that, in 1915, Captain O.H. Robertson of Harvard Medical School successfully demonstrated that blood could be safely transfused to wounded soldiers. He developed the transfusion bottle and pioneered universal donor blood, but the medical profession remained unconvinced.
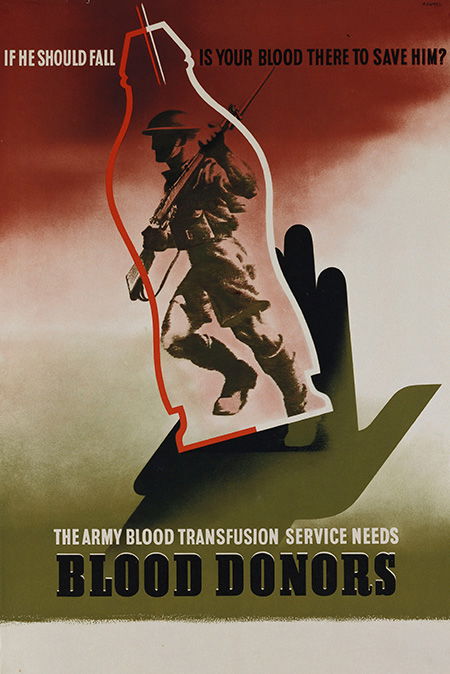
A London librarian, Percy Lane Oliver, along with his wife, carried out a number of altruistic acts. Having been impressed by a voluntary blood transfusion carried out in London’s King’s College Hospital, he was inspired to set up a volunteer panel of blood donors in 1921. This eventually led to the creation of the British Red Cross Blood Transfusion Service.
It was not until the Spanish Civil War, however, that large-scale blood transfusion became a real possibility, with the developments credited to Frederick Durán-Jordà and Henry Norman Bethune. The Spanish Civil War was among the first conflicts to result in widespread targeting of the civilian population and Durán-Jordà established a blood transfusion service in Barcelona in 1936, bringing blood to the front lines for transfusion to both soldiers and civilians. He was exiled to the UK after the Civil War (having been on the losing Republican side) and worked with Janet Vaughan at the Royal Postgraduate Medical School at Hammersmith Hospital, only to die from leukaemia at the age of 51.
Bethune, his contemporary, was a Communist Canadian surgeon, invited by the Committee to Aid Spanish Democracy to bring a surgical team to Madrid in 1936. In a similar fashion to Durán-Jordà, he recognised the importance of bringing blood to wounded soldiers and civilians rather than undergoing the lengthy process of transporting them to hospital for transfusion. He eventually returned to Canada, where he continued to raise money for the Spanish Republican cause, before emigrating to China, where he joined the Eighth Route Army during the second Sino-Japanese war, when he worked with Mao Zedong. He died of blood poisoning in November 1939, following surgery on an injured Chinese soldier.
During the Second World War, Vaughan worked with the Medical Research Council to establish blood donor centres in London. The provision of large-scale transfusion was vindicated not only at the retreat from Dunkirk but also during the Blitz, when it saved many lives, largely civilian.
In order to help the war effort, a campaign called ‘Plasma for Britain’ was established in the US. It was directed by Charles Drew, who fought to prevent the Red Cross from labelling the blood of African-Americans so it could not be transfused into ‘white’ soldiers. He was unable to overcome this prejudice, but ultimately his campaign was a success and the racial origins of donor blood are now kept confidential.
The main stimulus to develop blood and blood component therapy in the US was the Japanese attack on Pearl Harbor. Edwin J. Cohn, a chemist from Harvard University, developed a method of manufacturing albumin, a soluble protein found in blood plasma, for transfusion, initially as a powder and later as a liquid, used in the treatment of shock. It was to prove particularly important in the Pacific war and saved many lives on the battlefield, where hundreds of thousands of units of albumin were transfused.
The development of the atomic bomb, which brought the Pacific war to an end, was to contribute, albeit indirectly, to the treatment of leukaemia, hitherto a virtual death sentence. A major effect of atomic fission is the generation of ionising radiation, exposure to which leads to death from infection or bleeding because of low white blood cell and platelet counts. Animals in Los Alamos had reduced blood counts following exposure to ionising radiation during the Manhattan Project as did people in Hiroshima and Nagasaki after the atomic bombs were dropped on those Japanese cities at the end of the Second World War. It was found, however, that they could be saved by the transplantation of bone marrow cells from an identical ‘donor’. The result of these observations was the acceptance of the existence of haemopoietic stem cells, which eventually lead to the development of stem cell transplantation as a therapy for leukaemia and related diseases. A ‘Pandora’s box’ of biological discoveries had been opened.
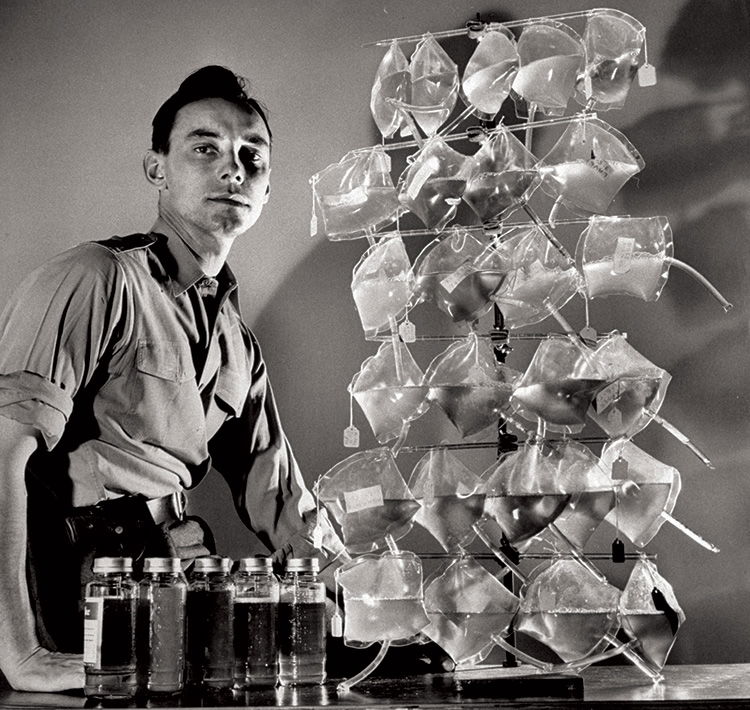
The interest in large-scale blood transfusion went into decline after the Second World War. Sometimes, however, what appears to be a simple invention can have long-lasting consequences, as was the case in the Korean War in the 1950s. The invention of a simple plastic bag led to a major development in blood transfusion. The bag had many advantages over the glass bottles that had previously been used to carry blood, in terms of weight, storage and transport. The first polyethylene blood collection bag had two tubes, one for blood collection and one to deliver blood to the recipient. It became widespread in the US in the 1950s, although it was not adopted in the UK until the 1970s.
Only comparatively recently has the lifesaving potential of blood transfusion been realised. War was undoubtedly the major force in the organisation of blood supplies and stimulated the development of new medical technologies. Research will continue, but will it always depend on war as its major stimulus?
Shaun R. McCann is Emeritus Professor of Academic Medicine and Haematology at St James’ Hospital and Trinity College Dublin. He is the author of A History of Haematology: from Herodotus to HIV (Oxford University Press, 2016).