Bad Blood?
Good intentions, misinformation and fear contributed to haemophiliacs becoming the hidden victims of HIV in Ireland.
They never saw it coming. In January 1985 the Irish Haemophilia Society (IHS) carried out an HIV screening for 133 of its members. It was a precautionary measure, as a haemophiliac child had been admitted to the National Children’s Hospital with AIDS-like symptoms. Of the 133 members, 54 were found to be HIV positive. More tests were held and the infections reached 112 – a third of the society’s membership.
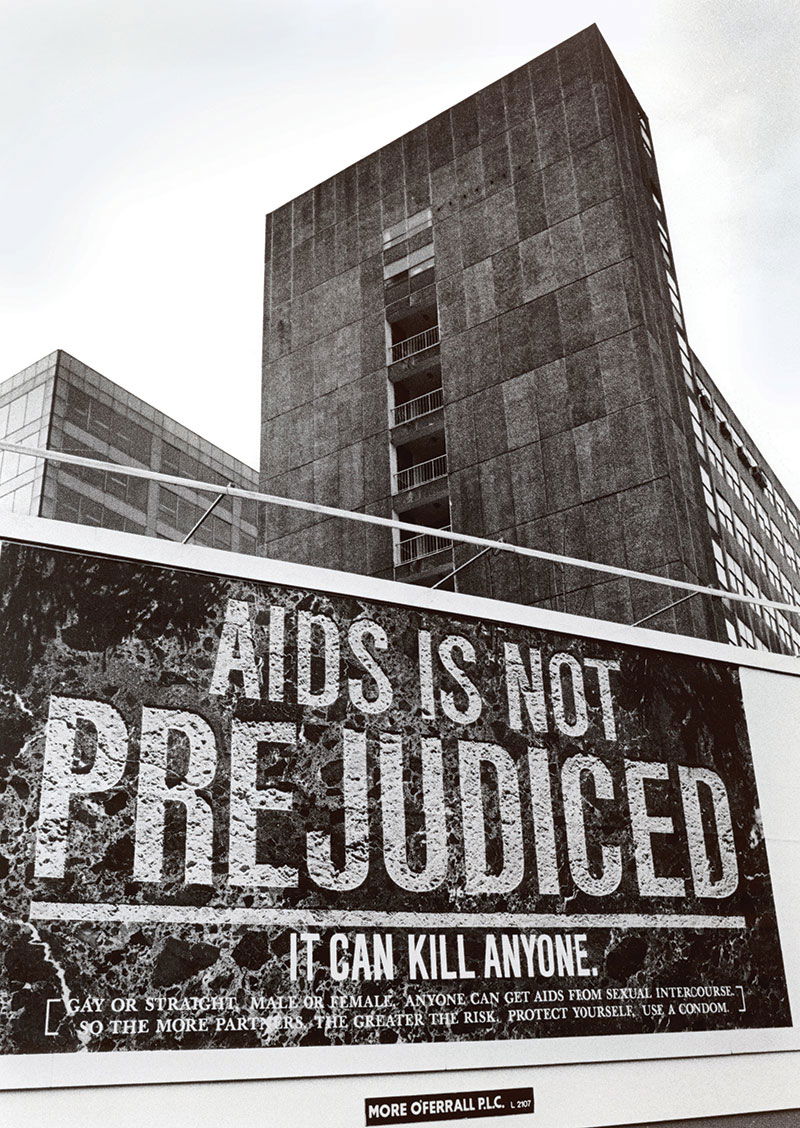
We know the old phrase that ‘History is written by the winners’. In some cases, this is true. But when it comes to HIV/AIDS, a story which offers no winners, the historical narrative has been shaped by the affected group that shouted loudest. In Ireland, this was the gay community, as activist organisations like Gay Health Action played a prominent role in educating the public about HIV/AIDS. This is, however, only a small fraction of a much messier narrative.